Stress and Movement
Movement.
Moving your body.
Do you do it? How often and what kind do you do? What kinds of movement are there?
In no particular order, let’s list just a few things as they come into my head …
Walking, running, sex, yoga, tai chi, weight lifting, boxing, self-defense, dancing, gardening, swimming, ball games, playing chasey, creating a snow angel.
Do you do any of these activities? Any different ones? Do you have a favourite?
Let’s talk about hormones again for a moment. You might remember some information about cortisol, one of the major hormones the body creates in response to stress. It’s the job of cortisol to calm the inflammation caused by stress. So in effect, to calm the stress response and help bring us out of it.
Many people find it helpful to go for a run when they feel antsy. Physical exercise helps burn off the energy caused by adrenalin. It reduces the urge to run away or fight, and helps us to relax. It can also help us to feel centred and to improve our mental wellbeing. It can lift our mood and reduce depression and anxiety.
However, we need to be careful. Exercise causes inflammation. The main job of cortisol is to reduce inflammation. So as you do more exercise, you produce more cortisol, which ultimately impacts your body’s ability to heal and reduce stress.
This cortisol production also leads to weight gain, particularly around the belly, face and neck. Now most of us, when we gain weight, tend to lean toward more exercise to reduce it, right? Can you see a pattern?
When you are already highly stressed, this will lead to a vicious cycle:
Intense exercise = cortisol production = weight gain = more exercise.
See the cycle?
For those of you who already struggle with your weight and believe the best thing you can do to drop it is to push your body to its limits, check out this video blog from a very well respected personal trainer who has experience with neuroscience and several other areas. Let me introduce you to Emma. I’ve been working with her for a couple of years and I trust her implicitly. She gets it. She knows what she is talking about.
So, when you are super stressed the best thing you can do is to go easy on the exercise. At least the exercise that is intense and of long duration. Let me be clear here. I’m not suggesting that you ditch your training. Nor am I suggesting that you become a couch potato. As someone who has been there, I can attest to the fact that the couch potato status can be just as stressful as the intense training.
There are types of movement that will support your body reaching the state of balance/homeostasis that Emma refers to.
Gentle movements such as tai chi, yoga or simple stretching will help. As will combining your movement with play. Have fun running around the yard with the kids. Throw a Frisbee together. Play hide and seek. Laugh together.
Relax.
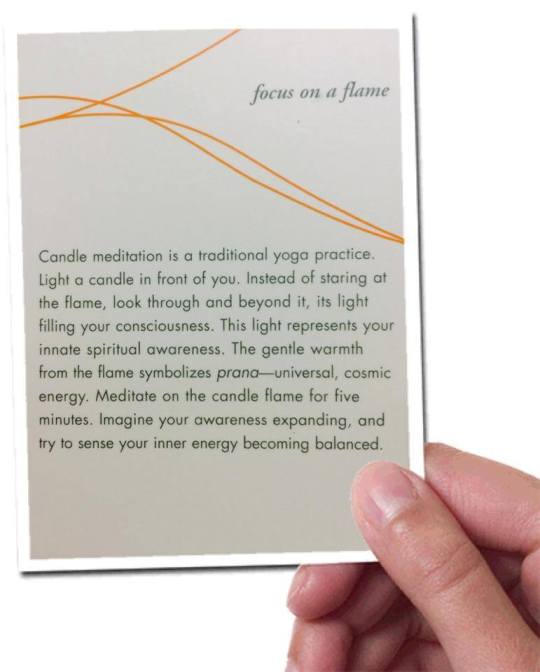
I’ve already talked about engaging the relaxation response to reduce stress. When Emma talks about taking her clients through a meditation activity at the end of her training sessions, she elicits this response, while at the same time, helping the brain to lock in new neural networks that reinforce the learning you’ve just done in training.
Ok. So now we’ve covered all that, let’s talk about how you can tell which type of movement you need to be doing.
Your body will tell you. So listen to the signals it gives you. Do you know what it’s saying?
Go with the urges that you get. If you have a feeling of deep down fatigue and the thought of getting out to exercise hard fills you with dread, it’s likely that your body is telling you it needs something different. If you feel the urge to get up and go hard, then by all means listen to that and take action to give your body what it needs. If you feel like dancing around your lounge with music at full volume, go for it!
Bottom line is this. Nobody can make up the rules for you. In any given moment your body will need different things to create and maintain that balance. Sometimes that means going full out and other times it means pulling back and resting. If you can learn the signals your body gives out, you will know what to do. How do you learn those signs? By listening to and connecting with your body.
Keep an eye out for a post on this soon.
As always, I’d love to hear from you, so please feel free to share your thoughts or questions below!