Reaching for the Light
This was posted on Facebook on August 13 by Kat Lambert and in my opinion it needs to be shared. Widely. It especially needs to be seen by those that live with depression and thoughts of suicide. It’s a long post so you might like to grab a cuppa and settle in. And it’s confronting, so be prepared.
If you experience depression and suicidal thoughts yourself, or have someone close to you that does, please pay attention. These are not things to be played with. They are serious and people need support to get through it! If you’re concerned about yourself or a loved one please reach out. Treatment is available! Either contact your mental health professional or if in crisis after hours, please call Lifeline on 13 1114 from anywhere in Australia.
—————————————————————-
I was somewhat reluctant to post this. Not because it’s something I am hesitant to share, but because a lot of other people are posting similar posts. Then I remembered the point of my post, being about breaking the stigma so people feel comfortable asking for the help they need to save their lives.
Obviously the suicide of Robin Williams has taken the world by surprise. How can this hilarious, wonderful human being, who has lit up our faces in lounge rooms and cinemas across the world, and made us laugh so hard that the tears have rolled down our face, have been in such a dark, depressing place that the only way out was for him to take his own life?
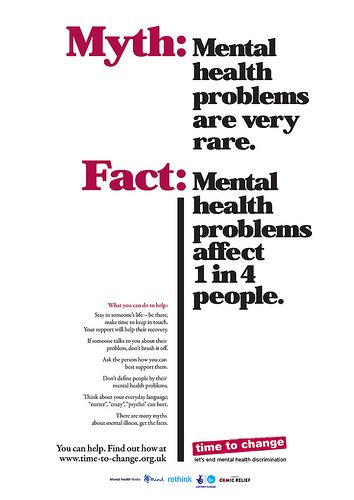
 And that’s just it. Depression, actually mental illness in general, affects people from all walks of life. Mental illness does not discriminate. Even those that seem the happiest, those that have the ability to light up the room with their enthusiasm, and those that seem to have it all can be fighting their own battles beyond their exterior facade.
And that’s just it. Depression, actually mental illness in general, affects people from all walks of life. Mental illness does not discriminate. Even those that seem the happiest, those that have the ability to light up the room with their enthusiasm, and those that seem to have it all can be fighting their own battles beyond their exterior facade.
Suicide is alarmingly, one of the highest causes of death in the world. Yet, unlike cancer, heart disease, SIDS, and other common illnesses where we raise awareness and we do everything we bloody well can to help our loved ones and the population in general, suicide is swept under the carpet.
Suicide is the “unknown”. People are scared of what they don’t understand. It’s easier to pretend it never happened, or to note the death of a loved one as “sudden” or “unexpected”. Because, God forbid, if you drop that “S” word into the conversation, guaranteed there’s always someone that has an opinion about it. So, on top of the guilt you already feel for not realising that your loved one was in such a horrible place, the guilt and the “what ifs” that run through your mind CONSTANTLY, you need to pretend like your son, your brother, your mother, your sister, died some other way, because otherwise people will judge you, and they’ll judge that family member, that friend, that you loved so dearly and couldn’t save. They’ll judge them for being weak, they’ll judge them for being selfish… And neither of these statements are true. It takes a fuckload of courage to step off that bridge, to pull that trigger, to swallow those pills, knowing that this will be the last time you take a breath, that you’ll never see your loved ones again, that once this has been done, it can not be undone. Once you’ve pulled that trigger it’s all over. Your decision is final.
Suicide is selfish. Are you fucking kidding me? Suicide is anything BUT selfish. Firstly, unless you’ve been in a place where you have not been able to see a way out, unless you’ve been in a place where nothing looks to ever get better, unless you’ve been in a place where you TRULY believe that your family would be less burdened if you weren’t around, then do NOT make assumptions that suicide is selfish.
How about instead of making ridiculous assumptions, we listen? We REALLY listen. Instead of judging people who constantly think about it, instead of judging those who’ve tried it before and failed, instead of making assumptions that these people are just screaming for attention… JUST LISTEN.
Listen to the people that have been there before, listen to those who have lost loved ones, listen to those who right this moment, need someone to listen. Listen to those who need someone, anyone, to tell them that life will get better. Someone to tell them that they are worth it, and that regardless of what they believe, the world would not be the same without them in it. Someone to hold them and tell them it is okay to NOT be okay.
to those who right this moment, need someone to listen. Listen to those who need someone, anyone, to tell them that life will get better. Someone to tell them that they are worth it, and that regardless of what they believe, the world would not be the same without them in it. Someone to hold them and tell them it is okay to NOT be okay.
And this is where the system fails. There are a very small amount of people in your life that you’ll feel comfortable opening up to when you’re in this state of mind. And even then, the information you give them is a lot less intense than those emotions, those thoughts that are running through your head. Then the guilt comes. “I’ve just burdened them with my problems. They have their own issues to deal with and I’ve just dumped all of my garbage on them. Maybe they’ll be better off without me. It’s not fair that I keep burdening them over and over again. At least if I’m gone, they won’t have to deal with the burden again and again. Sure they’ll be upset for a small while, but once the initial grieving to deal with my death is over, they’ll go back to their normal lives, and won’t have to worry about their crazy sister, daughter, friend. And I won’t have to feel this pain any more.”
I wish I could say that I’d never had thoughts like that. I wish I could say that I’d never even contemplated taking my own life. But I can’t. I have had thoughts like that, for many years at a time. And there was a time where it felt like suicide was my only option. I became ridiculously close to losing my life, and on more than one occasion.
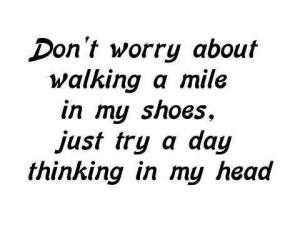
Seeking help wasn’t always an option. The ironic thing is that if you present at Emergency telling them that you don’t trust yourself to control your suicidal urges at the moment, they’ll shrug it off and tell you that you’re just looking for attention, and to take these sedatives, go home and sleep it off. That courage that you worked up for the previous three hours has been crushed in a matter of seconds. That last hope of help you managed to reach out for, has been thrown in your face. And right then, you make that decision that if you can’t go to a health professional for help, clearly you can’t get help anywhere. The drugs they give you to take home may assist you in sleeping off this period of inability to give in to the urges to take your own life. But next time, and most times, there is a next time, you think about taking yourself to Emergency, you think about reaching out for help, but then you remember last time. You remember the shame you were made to feel, those feelings of little importance, and judgment. So instead of reaching out your hand for help, you reach out your hand for that bottle of pills, for that gun, for that rope, and you truly believe that this is your only way out of the hell that exists inside your head.
them that you don’t trust yourself to control your suicidal urges at the moment, they’ll shrug it off and tell you that you’re just looking for attention, and to take these sedatives, go home and sleep it off. That courage that you worked up for the previous three hours has been crushed in a matter of seconds. That last hope of help you managed to reach out for, has been thrown in your face. And right then, you make that decision that if you can’t go to a health professional for help, clearly you can’t get help anywhere. The drugs they give you to take home may assist you in sleeping off this period of inability to give in to the urges to take your own life. But next time, and most times, there is a next time, you think about taking yourself to Emergency, you think about reaching out for help, but then you remember last time. You remember the shame you were made to feel, those feelings of little importance, and judgment. So instead of reaching out your hand for help, you reach out your hand for that bottle of pills, for that gun, for that rope, and you truly believe that this is your only way out of the hell that exists inside your head.
Then, after all this, if you’re lucky enough, you’ll end up in Emergency. You’ll be faced with those same nurses and doctors who made you feel ashamed because of your thoughts and feelings. Those who judged you and continue to judge you, those who turned you away, because your illness wasn’t real, and there were patients who NEEDED this service more than you did. If you thought that they’d understand now and things would change, think again. Now you’re the idiot that tried to kill herself when all the other people in Emergency are fighting for their lives. That patient next to you has been in a car crash, and is not expected to last the night. And here you are, distracting them from attempting to save the life of someone who doesn’t want to die. At that moment, the moment you notice their disgust, the moment you feel the shame that has been forced upon you, you make a decision that next time, you won’t fail and you won’t end up back here.
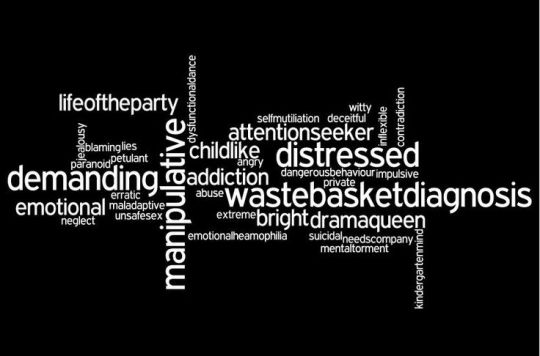
And that is where the problem lies. In our society, even though the stigma around depression has greatly decreased, suicide is still so much, a taboo subject. Clearly, like any illness, there are varying levels of symptoms, and whilst telling your friends that you’ve been depressed, and haven’t been able to eat and sleep is a fine conversation to have, if you dare mention that “S” word, if you dare mention how bad it is for you and how much suicide crosses your mind in a day, prepare to be judged. If you mention that the reason you can’t sleep at night, is because you can’t stop thinking of ending your life. The reason you can’t eat, is because you feel physically sick from the constant suicidal thoughts running through your mind. If you dare mention these things, you’ll be labelled as an attention seeker who is exaggerating your illness. You’ll be made to feel shame, on top of everything else you’re already feeling. And as such, any attempts to reach out for help, will be no more.
Sure, we can just continue to pretend that suicide doesn’t happen. We can pretend that nobody thinks about it. And that there’s nothing we can do to stop people anyway. But where’s that going to get us? Where will we be in 20, 50, 100 years’ time? At exactly the same place we are now. At the exact same fucking place where it is not okay to reach out for help. At the exact same fucking place where we constantly lose loved ones to something that could have been prevented. At the exact same fucking place.
So why don’t we do something about it? I don’t believe human kind can all be so stupid to believe that the current way is working. Talking about suicide doesn’t make people decide to attempt suicide, any more that talking about cancer gives people cancer. Talking about cancer, allows people to look out for the signs, and limit the severity if they notice them. Talking about suicide will do the exact same. Talking about suicide will bring it out of the shadows. Talking about suicide will mean that the person consumed with suicidal thoughts and feelings won’t feel ashamed about talking about it. That the person in this state, won’t feel ashamed to reach out for the help they so desperately need. Talking about suicide will mean that the stigma will be reduced, and when your mother, your child, your dad, your best friend, get to a point where they don’t think they can go on any longer, they will be able to reach out for help. In that split second, the fact that they can reach out for help without feeling ashamed, will save their life. In that split second, that very fact, will save you from heartache of losing someone you love so much and never understanding why. That split second, will save you from feeling such guilt and wondering if there was something you could have done differently, wondering why you didn’t figure out how bad it was for them, wondering “if only” for the rest of your life.
I’m not going to make out it’s an easy task, let’s face it, this is huge. This is massive. This is going to take a tremendous amount of funding. The Government is going to have to step it up a notch so that people can afford help. The Government would have to ensure that help was available to those in need, as so often, too often, patients are turned away due to a lack of available beds. But isn’t it worth a try?
Keep turning your back on suicide, and sweeping it under the carpet if you like, but what you’re really doing is turning your back on loved ones and judging, dismissing their feelings. I’m not telling you have to change your way of thinking, all I’m saying is, at some stage in your life, you’re likely to have a close friend or family member take their life, or at least attempt it, and in that moment, I want you to remember the decision you made right now, to keep this under the carpet. The decision you’re making, which means that your friend and family member hasn’t been able to source the help they need.