Stress and Trauma
Day 11 of our series on stress.
Wow, it feels like we’ve done heaps in such a short amount of time! But there is still so much to cover that it also feels like it will take forever to reach the end of the month! I have faith that we’ll get there though. We’re a resilient lot, really! We’re almost half way through the month and if you’re reading this, I’d like to thank you for sticking with us and hope you’re enjoying the series.
Today is all about trauma. Like we did in the first few days of the series, it’s probably a good idea to define what we’re dealing with here. So, according to the free dictionary, trauma is a noun:
-
- A body wound or shock produced by physical injury, as from an accident.
- The condition produced by this.
- Psychiatry. Psychological shock or severe distress from experiencing a disastrous event outside the range of usual experience, as rape or military combat.
- Any wrenching or distressing experience, esp. one causing a disturbance in normal functioning.
When I read this definition I am reminded of the simple definition that we learned about earlier in the month – stress is a force, pressure or strain.
Though it seems like it is an extreme form.
So, I’m going to connect the dots for you here and state that trauma is an extreme level of stress.
Like we did with our definition posts, let’s explore those things that create trauma. You’ll notice that many of the things on this list were also on the lists for physical, mental and emotional stress.
- Abuse – physical, sexual, emotional/mental, financial etc
- Bullying
- Car accidents
- Medical crises
- Muggings
- Physical fights
- War
- Yelling
- Injury
- Pregnancy or birth difficulties
- Illness or medical crisis
- Rape
- Animal bites
- Poisoning
- Seeing a distressing news article
- Drug taking
- Watching a distressing movie (I won’t go near horror movies for this reason!!)
- Witnessing someone else experience trauma
- Hearing a story about someone else experiencing trauma
I’ll come back to these final two items as they deserve special mention.
Once again, this list is not exhaustive in its content. There are plenty of other items that need to be added but right now my brain isn’t providing me with what I need. And like stress, trauma is a very individual experience. One person will be impacted by watching a specific movie and another won’t. One person will be impacted by witnessing a car accident and another won’t. There are a lot of factors that come into play.
I feel that the majority of it comes down to the neurobiological stress response that we have already discussed in several posts. We introduced it with Stress and the Triune Brain and continued it with Stress and the Amygdala.
If we’ve identified that trauma is an extreme stress response, doesn’t it make sense that its impacts also come from the stress response?
Except that since trauma is an extreme level of stress, so too are the impacts. In addition to those mentioned previously, people who have been traumatised may also experience items from this list, which has been taken from the Beyond Blue site.
- Re-living the traumatic event – The person relives the event through unwanted and recurring memories, often in the form of vivid images and nightmares. There may be intense emotional or physical reactions, such as sweating, heart palpitations or panic when reminded of the event.
- Being overly alert or wound up – The person experiences sleeping difficulties, irritability and lack of concentration, becoming easily startled and constantly on the lookout for signs of danger.
- Avoiding reminders of the event – The person deliberately avoids activities, places, people, thoughts or feelings associated with the event because they bring back painful memories.
- Feeling emotionally numb – The person loses interest in day-to-day activities, feels cut off and detached from friends and family, or feels emotionally flat and numb.
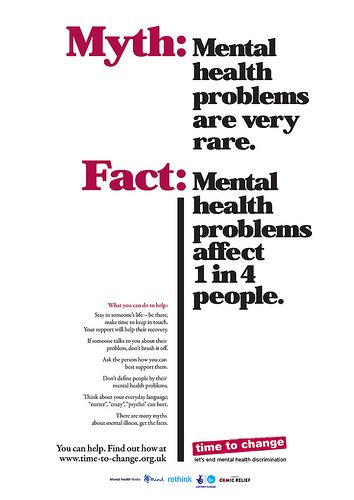
You’ll notice that some of these items are the same as those we came up with for stress, while others are different. One of the key things to remember about traumatic experiences is that these reactions are an absolutely normal response to a horrid, not normal event (or series of events). And it is possible that these responses can persist for a long period of time and can be diagnosed as Post Traumatic Stress Disorder.
This is a serious mental health concern that can be treated, and yet often isn’t due to stigma and a fear of being thought of as weak. If you have been traumatised and recognise these symptoms as things you have experienced, please, please, please seek support from a medical or mental health professional. And if you come across a professional who doesn’t want to know, find another one who is willing to listen. If you know a friend or family member who has been exposed to trauma and who is not receiving any support, please encourage them to read this post.
It’s important that everyone understands that this response comes about from the violation of our in-built, biological need for survival. It’s not something we can control. That sense of safety can be regained – with support from professionals who understand where it comes from and who have the skills to treat it. If you or someone you know needs some guidance on finding professional support, you can email me at mindseteffect@optusnet.com.au
One more note I’d like to make here. Trauma doesn’t have to be experienced to occur. Witnessing it or simply hearing about it can produce the same results. It’s real and it has a name – vicarious trauma. Many emergency personnel and mental health professionals or those in other helping professions (nurses, social workers, doctors etc) experience it, as do family members caring for someone with a disability, illness or mental health condition. There is support available.
I’d like to leave you with one final thought. There is no shame in reaching out for help.
Warning: If reading this post triggers your stress response, please consider seeking support from your team of professionals.