Please join Kaye as she shares her story of living with Borderline Personality Disorder and other mental health concerns. Please be aware that her experiences may trigger some emotions for you as you read her story. If you find yourself triggered, please take care of yourself and seek support. If you need to talk with someone please call Lifeline on 13 1114.
———————————————————-
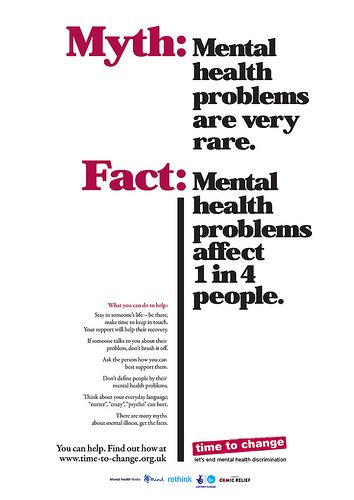
My name is Kaye and I am a 38 year old married mother of 5 beautiful girls. Like most people, I have a story, one that I am not always proud of but it is mine just the same. Also, like many people, my story involves a long term battle with mental illness, suicidal ideologies and self-injurious behaviours. In the hopes of reaching one person and making them feel that they are not alone, I would like to share my story with you all.

My childhood consisted of a rather insecure family unit, my father died in a tragic accident just after my third birthday and my mother never really recovered from this which left her looking to fill her own void, and in doing so she never really noticed how affected I was by the instability of my family or that I desperately craved her attention and affection. My mother eventually settled down with a man who was wonderful to both her and us kids, however this all changed when they had a baby girl who passed away at six weeks old from SIDS. From then on, my stepdad would beat my mother severely and he would do it in front of us. This continued from the time I was about 7 years old right up until I was about 14 years old. My stepdad decided at that point, that for things to change, he had to leave as my mother would not leave him because she loved him.
I thought that this event would make my life better, but it did not… in fact it got worse. I was constantly feeling hopeless, helpless, worthless and sad to the point that I began to see suicide as my only way out. I also began to burn myself with cigarettes to try and squash the emotional pain and replace it with physical pain. I pushed away all the friends that I used to enjoy being around, I stopped going out or leaving the house, I couldn’t eat and I slept endlessly but still felt tired when I did get out of bed. I started seeing a psychologist and was given numerous medications by numerous doctors, so I used them alongside alcohol to slip into that beautiful world of carefree serenity, where the pain and the hurt could not intrude.

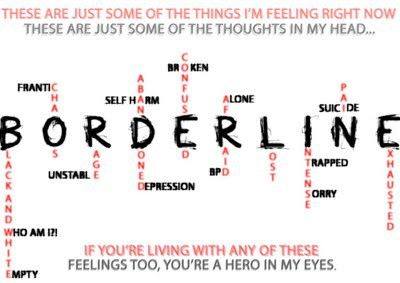
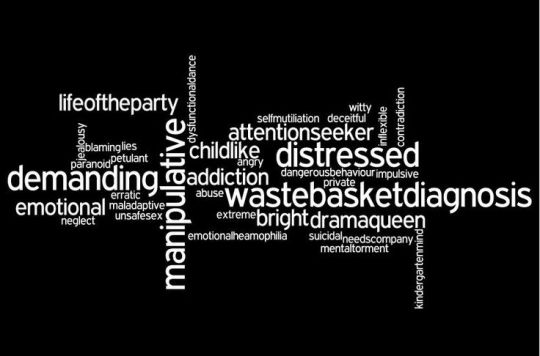
Naturally it didn’t take long before my first suicide attempt because I found that I needed more and more medication to reach that happy place. It was all just too much. This little venture landed me in a psychiatric unit on a 72 hour court order, for observation and investigation. I hated the hospitalisation but there was also a sense of relief for a while, relief that I was safe from myself and the demons that seemed to be growing stronger inside me every day. I was released two weeks later and continued to see my regular doctors as well as a psychiatrist who prescribed me much more medication! I was having the time of my life slipping in and out of consciousness on the chemical cocktails I was provided with. Eventually after ending up back in the psychiatric unit after another suicide attempt, I was diagnosed with what was called manic depression and borderline personality disorder with dissociative tendencies. I had no idea what this meant and I honestly did not care, all I knew is that I was getting worse and nothing  seemed to help me.
seemed to help me.
Eventually I married and had 2 daughters but the marriage lasted less than a year and I was devastated. Now I was on my own, battling the breakdown of my marriage, my own monsters were rising up to greet me again and on top of that, I was responsible for two little girls. I tried so many things to squash the bad thoughts and desire to self-harm and over medicate. I tried working but I couldn’t get out of bed. I found that socialising was too demanding and extremely tiring; I just wanted to curl up into a ball and die. Then I decided to try study but I couldn’t concentrate and pulled out with only one module left to complete a diploma in counselling (yeah, ironic huh?). No matter what I tried, I found a reason not to follow through with it. My ability to self-sabotage appeared to be endless. Again I fell back into old habits and began to over medicate and self-harm. But I did manage to quell the urge to attempt suicide.
When my girls were 5 and 7, I remarried. I found a man who seemed to be everything I had always wanted in a partner, he was honest, caring, reliable and he had the same values and beliefs around marriage and commitments as I did. The honeymoon didn’t last long though, our relationship became volatile and there was so much fighting, name calling and eventually physical threats. However, I hung in there, determined to make it work because I didn’t want another failed marriage and I desperately loved him. My instability began to show again and the old habits returned in spades, adding to the stress on our marriage. On top of this the 3 daughters I had with my husband all had special needs and one in particular was very difficult to handle. Again I started drinking and over-medicating so it was no surprise when I was admitted to the psychiatric ward again. This time I was determined to make the most of it and sort myself out. Luckily I was being treated by a psychiatrist who really looked at my mental health history and took the time to study what I was doing and what he could do about it. When I was released, he arranged for my medication to be supplied to me on a weekly basis from my chemist and he also kept in close contact with them to make sure that I was picking it up regularly. This man really cared about getting me on track and keeping me there. Things seemed to pick up a little after that. My demons still stirred but I finally had a doctor I trusted and who I believed could help me. I also found that I had a growing support network for my kids’ special needs, which helped all of us to cope.
A few years later I suffered what my psychiatrist said was a psychotic break after my marriage hit the rocks in a big way. I don’t recall what happened or anything that I did, but I ‘came to’ in hospital with both my arms bandaged from wrist to elbow and 2 police officers guarding me. This resulted in almost 3 months in the psychiatric unit and over a dozen doses of ECT. I was well and truly a mess this time and my demons were having a ball. It felt like my mind had split and I was two people fighting with each other inside my own head, one trying to tell me to keep fighting and the other telling me to just succumb to the endless abyss of what I am sure was insanity. It is difficult to put into words what I felt or thought but the one thing I can say is that I was so close to giving up and letting the darkness swallow me forever. I had nothing left; I was so empty and was in constant pain. I didn’t want to leave the ward, I didn’t want visitors and if the phone rang, I just let it keep ringing. Social interaction was just too much, even having to exchange words with the staff and other patients was exhausting. I think it’s fair to say that that was the lowest and blackest point in my life.
Eventually I returned home to try to resume some semblance of a life, but I wasn’t living, I was simply surviving. It took me a while to realise that surviving for me at that point, was living. If I didn’t focus on surviving I would end up dead, so I just kept surviving from one day to the next. My husband and I continued to try and work through our marriage and we kept going but things were never the same and neither was I. It is now just over 2 years since that breakdown and I am still surviving, one day at a time and sometimes one hour at a time. My demons constantly lurk in the recesses of my mind and I still have the eternal inner battle with myself over living or dying. I continue to take my medication and see my psychiatrist and psychologist regularly. With their firm support and the overwhelming love my family and friends have given me, I have redefined my life and have set myself some goals and a back-up plan for when things get rocky. I am currently studying a university degree in human services and I struggle with it every single day. Not just the workload but with the urge to self-sabotage because I feel that I am not worthy of doing something with my life. Whenever I think about throwing in the towel, I think about why I am doing this. I want to help others like myself who may not be as fortunate as I was in finding a support network that works, or someone that cares. I want to make a difference to them and help them to see that they are worthy and they can be and do whatever they want to do. Everyone deserves that and I intend to tell them so!
Mental health has seeped into every aspect of my life; personal, social, occupational and otherwise. I think the scariest thing about my illness is how my own mind can and has, betrayed me. This demon has twisted my thinking, taken my self-respect, left me powerless and torn me to pieces but it has also given me something. It has given me strength and purpose. No matter how vicious my illness has been, it has not beaten me yet and I am determined not to let it.