Stress and Sleep, Part 2
Today Linda is back to cover part 2 of her 3 articles on stress and sleep. Today she will discuss why sleep is so important and its relationship with stress. Remember yesterday, she talked about the sleep cycle and some technical aspects of how the brain processes it. While this information is a little technical, it’s important stuff to know so that you can then learn how to regulate your sleep. If you have any questions or comments to share, I’m sure Linda would love to help me address them for you! Hope you enjoy.
—————————————————————–
Why do we need sleep?
As you saw in the explanation of the sleep stages above, the simplest way to think about why we need sleep is in terms of healing and repair. It’s almost as though getting a good night’s sleep is akin to regularly taking your car into the mechanic for servicing. While you are sleeping your brain becomes a mechanic, tinkering with processes that are important during your day-to-day functioning and require fine-tuning or repair.
For example, any damage to your heart or blood vessels is repaired while you are sleeping. Hormone production, metabolism, cognitive functioning and immune function are all processes that rely on a healthy night’s sleep, every night. Physical growth and the stimulation of new brain cells and neural networks take place while you sleep.
Sleep is actually a very involved process. If you are interested in understanding more about the sleep cycle I came across one of the most detailed and interesting descriptions here:
https://science.education.nih.gov/supplements/nih3/sleep/guide/info-sleep.htm
How does stress impact on sleep?
In an earlier post titled ‘Stress Hormones’ you learned about a very important part of your brain directly responsible for many of the processes in your body including your immune functioning, your mood levels and emotions, your digestion, your energy production and storage, your sexuality, and the stress response. This system is known as the hypothalamo-pituitary-adrenal axis, or HPA axis. You may like to go back to this post and check out the diagram explaining the functioning of the HPA axis.
Sleep only occurs when the HPA axis is calm and inactive. So when the HPA axis is active, as is the case with stress, sleep will be affected. And conversely, when you don’t sleep well, the HPA axis becomes activated. And on it goes.
When the HPA axis has been activated through ongoing stress, you are also more likely to wake either through the night or first thing in the morning feeling anxious. I have met many people who have described waking in the middle of the night or early mornings with panic-attacks, and a disturbed sleep cycle could explain why.
So already we are beginning to see how disturbed sleep can trap you into a negative cycle: you don’t sleep well, you feel stressed. When you feel stressed, your biological clock becomes disrupted and you struggle to sleep well.
This process occurs in part because when we don’t get enough sleep (less than 6.5 hours) our body increases it’s production and release of the stress hormone cortisol. Remember from previous posts that when you are experiencing ongoing stress your body is already pumping out excessive levels of this toxic substance. Usually in the early evening cortisol is decreasing however with chronic sleep loss these levels will elevate resulting in a chain reaction including increased insulin resistance and decreased glucose tolerance.
Sleep is actually really important for regulating appetite and food intake. One of the hormones, letpin, which is responsible for appetite suppression, actually decreases with a lack of sleep. At the same time the body increases it’s production of ghrelin, a peptide that stimulates appetite. This means that when we experience disturbed sleep our appetite actually increases and we are more likely to eat larger amounts of food than what we would normally need to get through a day. We are also more likely to crave foods that are high in carbohydrates. Increased cortisol makes you store fat in your tummy, your neck and your face, so if you are eating more carbohydrates you are more likely to gain weight. A spare tire belly is a good indicator of stress, and for many of us it creates further stress as we begin worrying about our weight gain.
Sleep deprivation has also been related to impaired glucose tolerance and insulin resistance. If you find yourself waking between 1am and 3am, a common feature of stress, it may be because your body is not using glucose properly and is signaling that you need to re-fuel already. This is why having a snack prior to bed can be helpful.
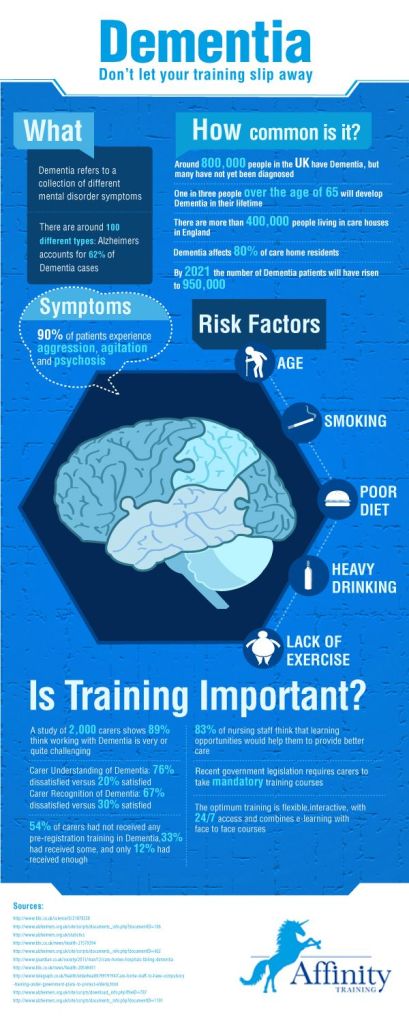
Even if you are young and relatively healthy, these hormonal changes can leave you in a pre-diabetic state following less than one week of sleep deprivation. This is an alarmingly short time frame! At the moment we are seeing an increase in sleep deprivation, an increase in diabetes, and an increase in Alzhiemer’s disease, which in some research circles has been labeled diabetes type 3.
Disturbed sleep can also leave you with confusion, impaired memory, headaches, impaired judgment and decision making ability, increased irritability, clumsiness, hallucinations, seizures, and even mania.
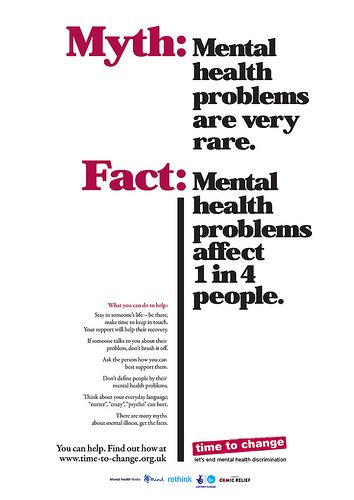
With ongoing stress and sleep disturbance your adrenal functioning may become impaired and this can be a factor in conditions like fibromyalgia, hypothyroidism, chronic fatigue syndrome, Cushing syndrome, arthritis, depression and premature menopause. Scary stuff! So what can you do about it?
Hang around and check out Tuesday’s blog post to learn how you can improve your sleep. As you can see, when you are stressed sleep is really the first step in attempting to help your system to down-regulate.
————————————————————-
 Linda is an AHPRA registered psychologist and relationship counsellor with offices located on the Gold Coast. She has worked in mental health since 1994. Since that time, following a long and often trying journey, particularly given that she had not completed secondary school, she achieved a Bachelor of Arts in Psychology, a Diploma of Counselling, a Graduate Diploma of Adult Education and a Post Graduate Diploma of Psychology. Linda now enjoys specializing in helping couples to learn how to value their best asset, enabling people suffering from dementia to move forward in their lives, and supporting people who have experienced work-place injury in their recovery. She also has a passion for assisting people to heal from stress, anxiety and depression.
Linda is an AHPRA registered psychologist and relationship counsellor with offices located on the Gold Coast. She has worked in mental health since 1994. Since that time, following a long and often trying journey, particularly given that she had not completed secondary school, she achieved a Bachelor of Arts in Psychology, a Diploma of Counselling, a Graduate Diploma of Adult Education and a Post Graduate Diploma of Psychology. Linda now enjoys specializing in helping couples to learn how to value their best asset, enabling people suffering from dementia to move forward in their lives, and supporting people who have experienced work-place injury in their recovery. She also has a passion for assisting people to heal from stress, anxiety and depression.
Linda values openness, authenticity, and acceptance in her work as a psychologist. She is a big believer in the power of the mind and recognizes that in many instances it is the activity within our minds that contributes to our psychological distress. Linda views the brain as an amazingly powerful organ: she is passionate about understanding how the brain functions and what each of us can do to maximize the brains potential.
You can find out more about Linda at www.eastqldcounselling.com.au.