Emotional Stress
Welcome to our third (and final) post in defining stress and really getting in and examining where our stress comes from.
Over the last two days we’ve discussed physical and mental stress and the types of things that influence them. On both days we’ve noticed a number of items on the lists that were a bit unexpected. I believe that today will be no different. There are many things that impact on our emotional stress. Emotions are fickle. They come and go with no rhyme or reason. Or at least we think there’s no rhyme or reason. The fact is, if we understand the mechanics of how our emotions work, we can often recognise the reason and therefore acknowledge where they originate. This of course makes them much easier to manage. So, keep an eye on our blog over the coming week for posts (that may be slightly technical) that will hopefully provide some insight for you.
So, let’s get down to our list. The formula we used yesterday and the day before seemed to work quite well, so following the same routine, we can deduce that emotional stress may be defined as anything that places pressure, strain or force on our emotions.
- Illness/injury (ever been cranky after stubbing your toe or walking on Lego?)
- Shock/accident
- Life challenges (marriage, death, buying a house etc)
- Work
- Parenting
- Beliefs
- Values
- Attitudes
- Seeing other people emotional
- Disagreements/fights with others
- Injustice
- Animals
- Relationships (partners, ex’s, kids, friends, colleagues etc)
- Finances
- Trying to fit in
- Keeping up with societies expectations
- Time – too much or not enough
- Success, procrastination
- Pleasing others
- Not having anything meaningful to do
- Others’ perceptions/opinions
- Not speaking your opinion/bottling up your emotions
- Threats to your life (either real or perceived)
- Abuse (physical, sexual, emotional)
- Criticisms/put downs
- Bullying
- Inability to do something (problem solving)
- Emotions (one emotion can trigger another or escalate what you’re already feeling)
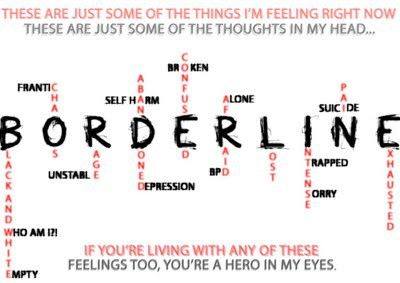
- Confusion
- Responsibility (too much or not enough)
- Thinking, ruminating or dwelling on problems
There are so many more things that need to be on this list and as I type my brain isn’t providing them. So I’m putting the call out for additions. Comment below and I’ll add them to the list.
The thing with emotions is that it is very easy for them to become overwhelming. Events trigger the emotion, you start thinking and ruminating on the event, which triggers more emotion. It becomes an uncontrollable cycle very quickly, leaving you feeling confused, overwhelmed and out of control. Not a pleasant place to be.
Think about this though. Our brains are pre-programmed to feel emotion. It’s a built-in survival system. Fear tells us when our environment is unsafe and we need to remove ourselves. Shock tells us that something has happened that our brain cannot process, so it helps to shut down the system for a while. And overwhelm tells us that our brains are a bit full and it needs a break to recover and process the things inside.
And given the fact that our current lifestyles continuously place more expectations on us, our brains and bodies really need something that helps us to manage everything.
The bottom line is this. Emotions are normal. Everyone feels them. They serve a purpose. And denying their existence just creates extra pressure that our systems need to manage, placing even more stress on us.