Love your body
So often we are bombarded by images and words about ugliness. We are lead to believe that we are inadequate and unworthy because of our appearance. We got (or get) bullied at school for wearing glasses or for having a few extra folds of skin and fat, or for having a birthmark on our face or for stuttering or for having stretch marks or … for a whole range of other things. We get bombarded by messages that say we MUST buy certain things in order to change who we are to be acceptable. Skin-care and makeup and surgery and clothing and accessories and whatever else you can think of.
We learn to hide ourselves from others and to fear being who we truly are. We become afraid of being judged and work hard to prevent it by buying into the messages we hear. We buy all the things we can to cover and mask ourselves. We cover up the small scar above our eye that told the story of when we fell off our bike at the age of 9. We get liposuction to rid ourselves of the fat that remains on thighs that have carried us through the hardest moments in our lives. We get our tummies tucked. Tummies that have carried precious children inside and allowed them to grow and to be nourished. Or tummies that tell the stories of how we have overcome years of abuse to be the healthiest we have ever been in our lives. We buy gym memberships to punish our bodies for being 5 kg larger than the person next to us. We buy gym memberships and hire personal trainers to smash us into the ground to rid our bodies of those extra 5kg. 5kg that protected us from the bullies or 5 kg that protected our babies or 5kg that enjoyed a little extra cake as we celebrated a major milestone in the lives of the people we love the most. Or 5kg that marks the journey of us mourning the loss of the person most important to us.
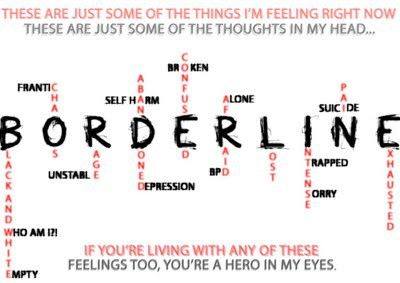
We do these things over and over and over again for years and expect to feel better about ourselves and the person we are becoming. We disconnect ourselves from the world. We disconnect ourselves from ourselves. Our mind becomes separated from our bodies and they operate independently. While we are busy cleaning or walking or whatever, our mind is busy thinking about how ugly we are or how inadequate we are or how we need the next best thing to repair the hole that was created 20 or more years ago.
The hole that nothing can repair. It seems that no matter what we try to do, no matter what we buy, no matter which gimmick we get sucked into, it doesn’t work.
You’re right. It won’t work. Because you don’t need a gimmick.
You cannot repair a hole, a disconnection between mind and body, with the next quick fix. You’re looking for a solution full of hate. A solution that is, in itself, flawed.
The idea of a quick fix (marketed to keep you buying products and designed to keep you feeling inadequate) repairing an emotional injury is ludicrous.
An injury of hate and inadequacy and unworthiness requires a solution of love, worth, and meaning. You need to feed the injury the emotions that it is missing.
There are no quick fixes that will ever work.
The only way to repair a disconnection is to reconnect. To get your mind and body talking to each other. To get them doing the same thing at the same time. Here are some key things I have learned about reconnection in my life.
- Acknowledge the story. Each “inadequacy” on your body tells a story about who you are. Those 5kg (or 10 or even 70kg) served a purpose
 at one point in your life. They may have protected your heart from the impact of abuse or they may have nourished and helped your children grow. Or maybe they supported you through years of grief. Your scars tell a story. Whether physical or emotional, the stories behind those scars have made you the person you are today. They got you through. They strengthened you. They supported you. To deny them is to minimize your spirit. To deny them is to say they mean nothing. And that is the furthest thing from the truth, when without them, you wouldn’t be who you are. So acknowledge the scars, whatever they look like. Send them love and gratitude for helping you get to today.
at one point in your life. They may have protected your heart from the impact of abuse or they may have nourished and helped your children grow. Or maybe they supported you through years of grief. Your scars tell a story. Whether physical or emotional, the stories behind those scars have made you the person you are today. They got you through. They strengthened you. They supported you. To deny them is to minimize your spirit. To deny them is to say they mean nothing. And that is the furthest thing from the truth, when without them, you wouldn’t be who you are. So acknowledge the scars, whatever they look like. Send them love and gratitude for helping you get to today. - Years of disconnect, abuse and hating yourself cannot be undone overnight. It takes patience and practice to reprogram your mind with messages of love, self-respect and support. So be patient with you. You deserve it.
- Surround yourself with a support team of people who believe in and practice unconditional acceptance. You deserve it. Include a team of professionals you can trust, to help you heal from the hurts. It’s worth it.
- Wean yourself (at your pace) from the quick fixes.
- Let go of any guilt you may have about needing the quick fixes. Even they serve their purpose. Sometimes they start you on your path back to connection and self-love. Mine have, and I am grateful that I had those tools at the time I needed them. It’s ok to need them; it’s ok to use them. When you no longer need them you’ll begin looking for new tools that will serve you moving forward.
- Send love to your body. Spend time regularly exploring it. Get to know it. The bumps, the bruises, the cellulite, the scars, the stretch marks, the bony bits. Run your fingers over your skin, observing the imperfections. Try to remain mindful of the experience. Remember the stories behind each imperfection. Forgive yourself. Love yourself. Pamper yourself. You deserve it.
- Use physical exercise to help you reconnect. When you’re walking, observe and feel the way your legs move. Feel the aches of being on your feet. Feel your arms swinging by your side. Observe the things around you. Notice the ground under your feet. Notice the path. Notice the flowers or the grass or the water or whatever it is you see. Observe your body as it navigates the terrain.
- Learn to listen to your body and what it needs. Learn the difference between the signals that say “I need to rest” and “I know you want to stop but that is your mind giving you false signals. Your body can do more and you’ll feel a huge sense of accomplishment if you can learn that you can do more than your mind thinks it can”.
One thing is certain in all this. You, and your body, are worthy. Worthy without conditions. You deserve unconditional love and acceptance, simply because you were born.
This video by Mary Lambert sums up this core message nicely.