Who cares for the carers?
People with mental illness usually have a support team around them. Psychologists, psychiatrists, mental health nurses, social workers, general practitioners. People in mental health organisations such as the Richmond Fellowship (this link is QLD but you can google other states). People handing out medications and people providing emotional support. For the most part, these people do fabulous work in paving the way to wellness.
But there is a whole other population that often gets overlooked. The family and friends. Husbands, wives, sons, daughters, mothers, fathers. The carers. They are often excluded from treatment due to “confidentiality”. How do carers help monitor medications if they don’t have accurate information about which prescriptions to fill or how many tablets are needed? How do they help regulate moods if they aren’t up to speed on which strategies have been used in therapy? And that also means they are unable to provide feedback to give the professional team a full picture of what is happening for their loved one. While I can’t speak for all carers, I know that the ones I have spoken to genuinely want to help support the road to wellness. And they want to respect personal space and privacy.
During periods of illness, carers are often confronted with some pretty tough stuff. Major mood swings. Irrational demands. Thought processes that aren’t based in reality. An inability to reason. Violence; to self and others. Hospital visits. Self-harm. Suicide attempts. Manipulation. Sometimes even homicidal tendencies. And they are often in the middle of the fray, caught up in the maelstrom of chaos.
Watching the people they love most in the world go through these experiences is heartbreaking. You watch your spouse with depression stay in bed day after day, week after week. You know that they are in pain and you try everything you know to help them. Encouragement, tough love, praise, cajoling, bringing friends in. You try talking to the doctors but you don’t get anywhere because they can’t talk back. You take over the running of the household, managing the children, cooking, cleaning. And you listen to your husband or wife talk about their inner pain and how much better off you and the children would be without him or her in it. You feel helpless and scared. What if they kill themselves? You wonder what else you can do to help. You don’t always understand why they can’t get themselves out of bed and rejoin the family. You feel lonely because the partner you knew isn’t there anymore. You feel alone because you don’t have your best friend to bounce things off. And you feel hopeless and helpless because the professional team won’t talk to you and tell you what you can do to help. Not to mention feeling guilty, fearful, resentful (of the illness), and a whole host of other emotions.
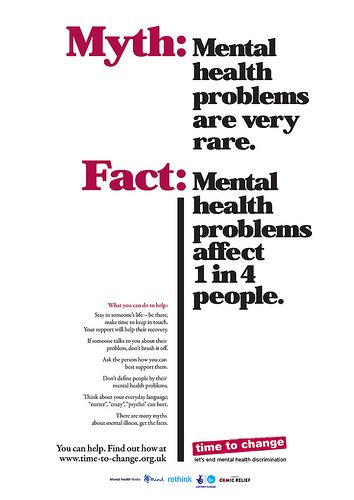
If you are a carer and can relate to this, please understand. You are not alone. There are hundreds of thousands, or even millions of people with mental illness, and each of them very likely has a group of family and friends around them, feeling exactly the same way you do. That is a lot of people feeling like you.
Exhausted. Stressed. Alone. Afraid. Confused. Helpless. Guilty. Isolated.
That is a lot of stress to deal with. And when you feel it for long periods of time, it is really important that you take care of yourself. Some very simple strategies can make a big difference in how you well you bounce back from the stresses and ultimately in the quality of your life.
When you’re looking at specific strategies there is one thing to keep in mind. Given the amount of stress most carers experience, sometimes thinking about doing extra can be overwhelming. So keep things really simple and you’ll be able to incorporate some of them into your normal routine. Try these:
- Take 3-5 long, slow deep breaths. Try to focus on slowing your breaths down and smoothing them out. This will get some oxygen into your brain and help you think more clearly.
- Pamper yourself. Take a bath, paint your nails, get a massage. This helps you relax your muscles and allows those stress hormones to dissipate.
- Surround yourself with nature. Visit a garden, sit under a tree, get your hands dirty with soil. This will help ground you and release the stress.
- Slow your brain down. Meditate, do yoga, or simply sit on your own for a while and breathe.
- Do something you absolutely love.
- Laugh.
- Connect with other people. Often speaking with other carers can help you realise you aren’t in this on your own and give you a chance to pick some brains about strategies that others have used successfully.
- Talk to someone. Sometimes seeing a professional can help you sort out the jumble in your head and give you some direction.
Australia has a network of carers organisations in each state that provide support for carers. They offer a variety of services, including access to support groups, workshops and counselling. They can also link you in with other services you may need. You can find details on each state’s organisation here, or call 1800 242 636 from anywhere in Australia. Some other countries also have carers organisations, including the UK and USA. Other support organisations in Australia include ARAFMI and COPMI (for the kids).